Published online Jul 18, 2015. doi: 10.5312/wjo.v6.i6.483
Peer-review started: February 27, 2015
First decision: April 27, 2015
Revised: May 20, 2015
Accepted: June 1, 2015
Article in press: June 2, 2015
Published online: July 18, 2015
Processing time: 138 Days and 18.2 Hours
AIM: To ascertain current surgeon practice in the United Kingdom National Health Service for the management of patients undergoing lumbar spinal fusion surgery.
METHODS: Descriptive survey methodology utilised an online questionnaire administered through SurveyMonkey. Eligible participants were all surgeons currently carrying out lumbar spinal fusion surgery in the National Health Service. Two previous surveys and a recent systematic review informed questions. Statistical analyses included responder characteristics and pre-planned descriptive analyses. Open question data were interpreted using thematic analysis.
RESULTS: The response rate was 73.8%. Most surgeons (84%) were orthopaedic surgeons. Range of surgeon experience (1-15 years), number of operations performed in the previous 12 mo (4-250), and range of information used to predict outcome was broad. There was some consistency of practice: most patients were seen preoperatively; all surgeons ensured patients are mobile within 3 d of surgery; and there was agreement for the value of post-operative physiotherapy. However, there was considerable variability of practice: variability of protocols, duration of hospital stay, use of discharge criteria, frequency and timing of outpatient follow up, use of written patient information and outcome measures. Much variability was explained through patient-centred care, for example, 62% surgeons tailored functional advice to individual patients.
CONCLUSION: Current United Kingdom surgeon practice for lumbar spinal fusion is described. The surgical procedure and patient population is diverse, and it is therefore understandable that management varies. It is evident that care should be patient-centred. However with high costs and documented patient dissatisfaction it is important that further research evaluates optimal management.
Core tip: This study surveyed all surgeons carrying out lumbar spinal fusions in the United Kingdom (response rate 73.8%) to ascertain current practice. Eighty-four percent of participants were orthopaedic surgeons and their experience of lumbar spinal fusion ranged from 1-15 years, each performing 4-250 operations in the previous 12 mo. Surgeons consistently saw patients preoperatively, ensured patients are mobile within 3 d of surgery, and valued post-operative physiotherapy. However, variability of protocols, duration of hospital stay, use of discharge criteria, frequency and timing of outpatient follow up, use of written patient information and outcome measures was considerable. Much variability was explained through patient-centred care.
- Citation: Rushton A, White L, Heap A, Heneghan N. Evaluation of current surgeon practice for patients undergoing lumbar spinal fusion surgery in the United Kingdom. World J Orthop 2015; 6(6): 483-490
- URL: https://www.wjgnet.com/2218-5836/full/v6/i6/483.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i6.483
In the United Kingdom, the largest single component of expenditure for the management of low back pain is surgery[1]. Lumbar spinal fusion accounted for 14% of United States back surgery expenditure in 1992, increasing to 47% by 2003[2]. Recent data evidences a worldwide increase in lumbar spinal fusion, illustrated by > 4036 operations within the United Kingdom National Health Service[1] in 2009/10[3]; representing a 14% increase on the previous year. The United States reported an increased spinal surgical rate of 220% from 1990-2001[4,5] followed by a reduction between 2002-2007, although during the same period the rate of lumbar fusion surgery increased from 1.3 to 10.9 operations for every 100000 patients[6]. The increased rates are partly explained by technological advances, including the United States Food and Drug Administration’s approval in 1996 of intervertebral cage implants and in 1998 of pedicle screws. Data also reveals considerable variation in fusion rates between regions within and between countries[2,7], suggesting poor surgeon consensus and/or a range of indications for surgery. A recent survey found a lack of consensus between 62 surgeons (Netherlands) regarding both prognostic factors and predictive tests for patient selection for surgery[8].
The primary indication for lumbar fusion is back and/or leg pain as a result of degenerative disease, as it can potentially help to stabilise the spine[9]. It is acknowledged that fusion could be beneficial in some patients but it remains a controversial procedure[8]. The updated Cochrane review investigating effectiveness of surgery for lumbar spondylosis of degenerative causes found conflicting results[1], and in the more recent United Kingdom spine stabilisation trial, there was no evidence that fusion was more beneficial at 2 years follow up compared to an intensive rehabilitation programme[10]. The trial also identified a higher complication rate than previous trials, and evidence of less cost-effectiveness for surgery when compared with intensive rehabilitation[10]. Swedish National Spine Register data illustrate that 40% patients communicated dissatisfaction regarding their outcome at 12 mo, and 25% patients had no change or described worsened pain (back and/or leg) following their surgery[11].
Synthesising existing literature, the increasing rate of surgery, lack of data supporting effectiveness of surgery, the high reported patient dissatisfaction, continued level of patient disability, documented high revision rate (in the United Kingdom > 200/year)[3], and 13% re-hospitalisation rate (United States)[6], evidence two problems. Firstly, research needs to investigate the effectiveness of fusion surgery in specific populations of patients, and, secondly, that optimal outcomes of surgery through post-operative management/rehabilitation requires investigation. Our recent systematic review[12] found only two trials, providing inconclusive evidence of very low quality for the effectiveness of physiotherapy rehabilitation for patients after lumbar spinal fusion surgery.
An initial evaluation of current practice by surgeons is necessary to ensure the appropriate focus and parameters of future trials. No evaluation of surgeon practice has specifically focused on lumbar spinal fusion. McGregor et al[13] did evaluate post-operative practice of spinal surgeons in the United Kingdom across the range of their surgical procedures; finding considerable variation in practice, inconsistent advice regarding functional restrictions following surgery, and limited referral for rehabilitation.
To ascertain current surgeon practice in the United Kingdom National Health Service for the management of patients undergoing lumbar spinal fusion surgery.
A descriptive United Kingdom survey[14] was conducted. Target settings were all units within United Kingdom NHS Trusts in which surgeons perform spinal fusion surgery; and, the aim was to obtain data from all surgeons who currently conduct lumbar spinal fusion surgery.
Data were collected through an on-line SurveyMonkey questionnaire to ensure participants’ cost effectiveness (ease of questionnaire return, response time), ease of administration (no paperwork, easy tracking of reminders and returns), and ease of data management[15]. At 3 and 6 wk, reminders were sent to participants.
A team consisting of a spinal surgeon, physiotherapists, and research methodologists developed the range of closed and open questions; informed by the findings from our recent systematic review[12], and previous surveys on spinal surgery[13] and lumbar discectomy[16]. The questionnaire consisted of 4 sections: surgeons’ backgrounds, surgical procedures, and pre- and post-operative practice. There were 2 phases to the pilot of the questionnaire. Phase I recruited student physiotherapists (n = 15). Surgeons were not used as it was predicted that the potential sample for the main study was limited. Phase II recruited physiotherapists working in spinal surgery and surgeons who would, then, not participate in the survey (n = 5). Sequencing and wording of questions were amended to enhance the questionnaire’s reliability and validity.
Data were downloaded to SPSS (version 19), and to ensure integrity were checked. None of these data were traceable to individual respondents. All analyses were pre-planned and comprised summaries across respondents, to ensure anonymity of findings. Statistical analyses incorporated a combination of simple graphical, tabular and numerical descriptive summaries of: characteristics of surgeons, variation in routine surgical practice pre-operatively and post-operatively. Open question data responses were analysed through thematic analysis.
The target population comprised surgeons currently performing spinal fusion surgery within NHS Trusts and major surgery centres. Recognised registers of surgeons (e.g., register of the British Association of Spinal Surgeons), and contact with all NHS Trusts, Health Authorities and specialist orthopaedic centres in the United Kingdom enabled the identification of surgeons. Cross-referencing of these sources created a listing of potentially eligible surgeons. Invitations to participate were sent through email accompanied by a Participant Information Sheet. This approach for recruitment was verbally approved by the local Research and Development office. Ethical approval was provided by the University of Birmingham. Questionnaire completion was taken as informed consent. To ensure that it was not possible to link data to individuals, IP addresses were not saved. The questionnaires were distributed to 42 eligible participants.
Thirty-one out of 42 questionnaires were returned giving a response rate of 73.8%. Twenty (64%) surgeons worked in a teaching/University hospital, 8 (26%) in a District General Hospital and 3 (10%) in a Specialist Centre. Of these, 1 surgeon worked across both a teaching/University hospital and Specialist Centre. Five (16%) surgeons who worked in a University/teaching hospital specialised in neurosurgery, whilst all others (n = 26, 84%) specialised in orthopaedic surgery. Experience in lumbar spinal fusion surgery ranged 1-15 years (median 10, inter-quartile range 4-17 years). The surgeons had conducted 4-250 fusion operations in the previous 12 mo = (median 23, inter-quartile range 20-40 operations). Nineteen (61%) surgeons reported no change in the rate of surgery based on their experience over the previous 5 years, whilst 7 (23%) reported an increase and 5 (16%) a decrease.
Of the surgeons reporting on pre-operative management (n = 30, 94%), their patients were seen pre-operatively by nurses (n = 21, 70%), anaesthetists (n = 19, 63%), physiotherapists (n = 13, 43%), occupational therapists (n = 2, 7%) and other healthcare professionals (5, 17%) (e.g., pain specialist). All surgeons discuss expected post-surgery outcomes with patients. One surgeon’s patients underwent a spinal rehabilitation programme pre-operatively. Surgeons reported a range of indications for surgery, that management should be tailored to the individual patient, and that patient factors (motivation, pre-operative fitness, weight) influence management decisions. Surgeons used a range of information to predict expected outcome (Table 1). Thirteen surgeons (43%) provided written information sheets/booklets for patients pre-operatively.
| Patient characteristics and history |
| Patient personality and expectations1, including motivation |
| Age, occupation/unemployment, social issues, smoking, weight |
| Presence or absence of personal injury or yellow flags |
| Diabetes, other medical co-morbidities |
| Clinical information including patient history, e.g., symptoms duration |
| Use of outcome data, e.g., DRAM, GAD7, ODI, PHQ9, SF36, SRS, VAS pain, walking |
| Response to previous approaches, e.g., physiotherapy, facet joint injections, discogram, disc block |
| Pathology or degree of deformity |
| Number of levels predominant leg pain; more leg than back pain |
| Performance based outcome measures |
| Neurological examination |
| Imaging: CT scans, CT with 3D reconstruction, discography, MRI scans, X-ray |
| Evidence |
| Audit of data from past patients |
| Literature or empirical evidence |
| Experiential clinical experience |
| Other |
| Pathology: segmental instability, single level, spondylolisthesis, central disc protrusion |
| Pain mechanism: no features of chronic regional pain syndrome (allodynia, non-anatomical pain), stenosis |
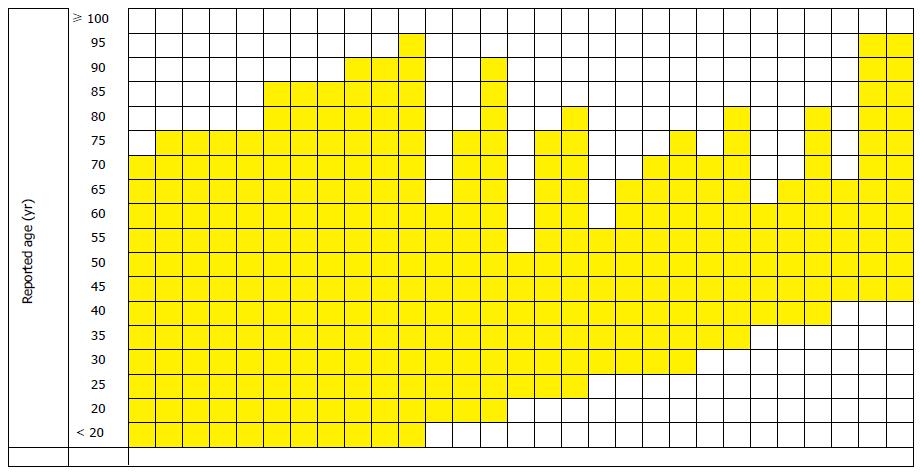
Twenty nine (91%) surgeons provided information regarding operations. Instability, leg and back pain were the most frequently reported indicators (Table 2). Reported ages of patients undergoing operation ranged 14-100 years (Figure 1), with variation in reports for the youngest (14-50 years) and oldest (55-100 years). Twenty four (83%) surgeons reported that the mean patient age had not changed over the last five years.
| Key indicator for surgery | Surgeons n (%) |
| Instability | 25 (86) |
| Leg pain | 21 (72) |
| Back pain | 18 (62) |
| Failed conservative treatment | 17 (59) |
| Failed previous surgery | 16 (55) |
| Degenerative disc disease | 15 (52) |
| Neurological changes | 13 (48) |
| Other1 | 12 (41) |
All surgeons (n = 29) reported using instrumentation for some operations, with 11 (38%) performing operations without instrumentation. Other variations, used by over half of the responding surgeons, included: open procedures (n = 26), posterior lumbar interbody fusion (n = 20), transforaminal lumbar interbody fusion (n = 20), anterior lumbar interbody fusion (n = 15), transforaminal lumbar interbody fusion (n = 20), combined anterior and posterior fusion (n = 13), and minimally invasive procedures (n = 15). Five surgeons reported other procedures that included: posterolateral fusion; posterolateral fusion with pedicle screws; posterior spinal fusion with instrumentation without anterior interbody fusion and posterolateral graft; transforaminal lumbar interbody; fusion cage inserted by posterior lumbar interbody fusion approach; and lateral interbody fusion. Surgeons reported that during the previous 5 years, 30%-90% of patients required fusion at 1 level, 10%-40% 2 levels and 10%-30% ≥ 3 levels.
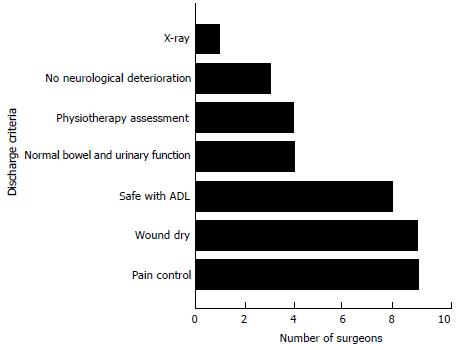
Twenty two (76% of 29) surgeons used post-operative protocols/pathway/discharge criteria. Nine surgeons reported that the protocol varied according to type of surgical procedure, with 5 reporting influence for anterior vs posterior lumbar interbody fusion, or instrumented vs non-instrumented procedures. Thirteen surgeons reported that the protocol was not influenced by procedure. Other reported factors influencing protocols included presence of co-morbidities, patient factors (fitness, weight), and speed of mobilisation. Written instructions/advice were provided post-operatively by 16 surgeons (55%). Post-operative physiotherapy was provided routinely to patients of 27 surgeons (93%); the remaining 2 surgeons would never provide physiotherapy. More than half of surgeons (n = 15, 52%) did not employ discharge criteria. Of the 14 (48%) who did, there was no consensus of medical and functional criteria being used (Figure 2).
A range of post-operative complications were reported by surgeons with persistent symptoms (n = 18, 62%) and dislodged instrumentation/implant failure (n = 14, 48%) most commonly reported (Table 3). In the absence of complications, all surgeons (n = 29) reported that patients are mobilised within 3 d of surgery, with the majority (n = 24, 83%) mobilised on the same or first day post-operation. Patient reported outcome measures are rarely used, with only 2 surgeons (5%) routinely using pain Visual Analogue Scale and Oswestry Disability Index, and 1 of these surgeons additionally using SF-12. No surgeons use performance based outcomes measures.
| Complications of lumbar spinal fusion surgery | Surgeons n (%) |
| Persistent symptoms | 18 (62) |
| Dislodged instrumentation/implant failure | 14 (48) |
| Infection | 9 (31) |
| Failure of fusion | 7 (24) |
| Dural tear | 6 (21) |
| Nerve injury | 5 (17) |
| Failure at adjacent level | 4 (14) |
| No improvement | 3 (10) |
| Other1 | 8 (28) |
Advice on return to function was tailored to individual patients by 18 surgeons (62%); dependent upon patient factors (age, fitness, occupation, expectations, compliance, motivation, anxiety levels), surgical factors (bone quality, quality of fixation), presence co-morbidities (obesity), complications and pain levels. Surgeons’ advice on when to return to sitting varied from immediately to 6 wk; return to driving, sex and work from 1 wk to 6 mo; and sport, contact sports, jogging/running, outer-range lumbar movements, heavy lifting and weight training from 2 wk to 9 mo (Table 4). Use of corsets was infrequent with 2 surgeons (7%) recommending, and 7 (24%) occasionally recommending use. Reason for corset use related to pain (n = 4), compliance with protecting back (n = 2), bone problems (n = 2), anterior lumbar interbody fusion (n = 1), multilevel surgery (n = 1), and in one instance it was standard practice to encourage mobilisation.
| Functional activity | No. (%) of surgeons | ||||||||
| Weeks1 | Months1 | ||||||||
| 1 | 2 | 3 | 4 | 6 | 8 | 3 | 6 | 9 | |
| Sitting | 22 (85) | 2 (8) | 1 (4) | 0 | 1 (4) | 0 | 0 | 0 | 0 |
| Driving | 0 | 4 (15) | 3 (12) | 10 (39) | 10 (39) | 2 (8) | 0 | 0 | 0 |
| Sex | 2 (10) | 3 (15) | 2 (10) | 6 (30) | 9 (45) | 2 (10) | 1 (5) | 0 | 0 |
| Work | 0 | 2 (8) | 3 (12) | 2 (8) | 13 (50) | 4 (15) | 9 (35) | 1 (4) | 0 |
| Sport | 0 | 1 (4) | 0 | 1 (4) | 4 (17) | 0 | 10 (42) | 6 (25) | 2 (8) |
| Contact sports | 0 | 0 | 0 | 0 | 0 | 0 | 5 (21) | 8 (33) | 2 (8) |
| Jogging/running | 0 | 0 | 0 | 1 (4) | 6 (25) | 1 (4) | 5 (21) | 10 (42) | 1 (4) |
| Weight training | 0 | 0 | 0 | 0 | 1 (5) | 0 | 5 (21) | 9 (41) | 3 (14) |
| Heavy lifting | 0 | 0 | 0 | 0 | 2 (8) | 0 | 5 (21) | 10 (42) | 1 (4) |
| Extreme range of lumbar movements | 0 | 1 (5) | 0 | 0 | 0 | 0 | 8 (36) | 6 (27) | 2 (9) |
Surgeons reported variability of duration of hospital stay for elderly patients, multilevel surgery, or different types of surgery. The majority (n = 20, 69%) reported that patients remain in hospital 1-4 d, with 8 (28%) reporting stays of 3-4 to 6-7 d and one surgeon reporting hospitalisation of 3-10 d.
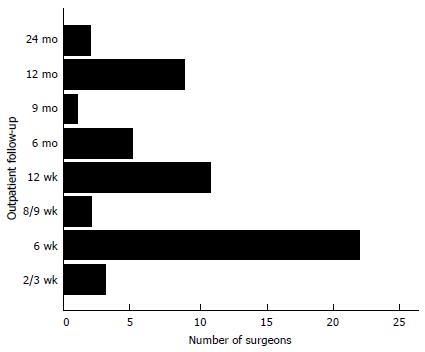
All surgeons (n = 29) followed up patients as outpatients although frequency and timing varied considerably from once at 3-6 wk (n = 15) to a maximum of five visits in once instance (at 6, 12, 24, 52 wk and 2 years) (Figure 3). Written information sheets/booklets were provided to outpatients by nine (31%) surgeons, with 20 (69%) not using standardised information sheets.
There was wide variation in use of patient reported outcome measures, ranging from no measures (n = 10, 34%) to 8 surgeons using ≥ 3 tools; and routine use by 19 (66%) surgeons. The ODI, SF-36 and a pain rating scale were most frequently used, with ODI and VAS most frequently used in combination. There was a diverse range of additional measures (Table 5). Performance based measures were only used occasionally by 2 (7%) surgeons. From open question data (n = 3) the need to monitor outcomes appears to be a current priority for implementation.
| Domain | Questionnaire | Surgeons n (%) |
| Disability | ODI | 17 (90) |
| Pain | VAS or NPRS | 14 (74) |
| MSP | 1 (5) | |
| Pain drawing | 1 (5) | |
| Health | SF-26 | 6 (32) |
| SF-12 | 1 (5) | |
| PHQ-9 | 1 (5) | |
| EQ-5D | 1 (5) | |
| Depression | Zung Depression Index | 2 (10) |
| Hospital Depression Scale | 1 (10) | |
| Anxiety | Hospital Anxiety Scale | 1 (10) |
| GAD-7 | 1 (10) | |
| Other1 | 2 (10) |
Outpatient physiotherapy is used routinely by 14 (48%) surgeons, or when required by 15 (52%). Indications varied based on medical or personal factors: ongoing pain or stiffness (n = 8), requirement for education or confidence building (n = 7), lack of progress linked to function (n = 4), poor trunk control (n = 3), on patient’s request (n = 1), following previous surgery, elderly patients, or patients finding rehabilitation difficult. One surgeon reported standardised care including 6 wk of hydrotherapy followed by gym exercise.
Surgeons reported a small percentage of patients requiring further invasive procedures: < 5% (n = 13, 49%), 10%-15% (n = 11, 38%), and 20%-25% (n = 1, 8%) of cases, with 1 reporting no patients based on their past 5 years of experience. Procedures included: adjacent level surgery (n = 20, 69%), removal of metal-ware (n = 17, 59%), same level surgery (n = 13, 45%), and injection at adjacent level (n = 19, 66%). Reported reasons from 6 (21%) surgeons included other spinal problems or symptoms, unrelated back pain or implant failure.
The 73.8% response rate was good. Most surgeons (84%) were orthopaedic surgeons, perhaps reflecting the mechanical nature of patient presentations. This contrasted our previous survey findings when investigating lumbar discectomy, where patients were managed equally by neurosurgeons and orthopaedic surgeons[16]. The range of surgeon experience (1-15 years) was broad, as was the number of operations performed in the previous 12 mo (4-250), and range of information used to predict outcome (Table 1); perhaps reflecting regional variation[2,7] and poor surgeon consensus and/or a range of indications for surgery and outcome[8]. In contrast to international data[1-6] surgeons reported no increase in surgical rates over the previous 5 years.
The findings illustrate some consistency of practice as most patients were seen preoperatively (94%) and the importance of this encounter was clear. All surgeons ensured that patients are mobile within 3 d of surgery, with most being mobile by day 1 (83%). There was also agreement for the value of post-operative physiotherapy that was provided routinely for inpatients of 93% surgeons, and for outpatients of 48% surgeons. Surgeons were consistent in reporting a small percentage of patients requiring further invasive procedures (0%-15% cases), in contrast to existing data[3,6].
Overall, there was considerable variability of practice in managing patients. Although most surgeons used protocols to guide management, there was disagreement regarding variability of post-operative protocols according to surgical procedure, but recognition that co-morbidities, patient factors, and speed of mobilisation did contribute to variation. Fifty-two percent of surgeons did not have specific discharge criteria, and there was no consensus for criteria when used. Sixty-two percent of surgeons tailored advice on return to function to individual patients, and surgeons reported variability of duration of hospital stay for different patients. All surgeons followed up patients as outpatients, but frequency and timing varied considerably. Surprisingly, in the current context of needing to evidence outcomes, use of patient reported outcome measures was limited and variable, and use of performance based outcomes measures minimal. It was not clear from the data whether surgeons see a distinction between patient reported and performance based outcomes, which considering the emphasis on function post recovery is an important consideration. Written support for patients was variable for inpatients and outpatients. This range of written support for patients can be improved to enhance patient care.
Several reasons perhaps explain the variability of practice. Firstly patient-centred practice was clear, with most surgeons advocating tailoring management to the individual patient. Secondly, the range of indications for lumbar spinal fusion was emphasised and this was also reflected in the range of surgical procedures, and number of levels fused, again dependent on the individual patient’s presentation. Thirdly patient factors were felt to influence management (motivation, pre-operative fitness, weight).
The strengths of this survey are its good response rate from a United Kingdom wide population. A key limitation is that the survey structure did not provide further information on clinical decision making from surgeons to manage the obvious variability of surgical indication and patient presentations.
A description of current United Kingdom current surgeon practice has been provided by this survey for managing patients both pre- and post-operatively when undergoing lumbar spinal fusion surgery. The surgical procedure takes many forms, and combined with the diversity (and possible complexity) of this patient population it is understandable that protocols and management approaches vary. It is evident that care should be tailored to the individual through patient-centred care. However with high costs and documented patient dissatisfaction[3,6,11], it is important that further research evaluates optimal management.
The Musculoskeletal Association of Chartered Physiotherapists for small funding to enable participant identification and access to SurveyMonkey software.
The increasing rate of lumbar spinal fusion surgery, lack of data supporting effectiveness of surgery, high level of patient dissatisfaction, continued level of patient disability, high revision and re-hospitalisation rate, evidence two problems. Firstly, research needs to investigate the effectiveness of fusion surgery in specific populations of patients, and, secondly, that optimal outcomes of surgery through post-operative management/rehabilitation requires investigation.
No evaluation of surgeon practice has specifically focused on lumbar spinal fusion. The objective of this study was to ascertain current surgeon practice for the management of patients undergoing lumbar spinal fusion in the United Kingdom National Health Service.
Current United Kingdom surgeon practice for lumbar spinal fusion is described. This study surveyed all surgeons carrying out lumbar spinal fusions in the United Kingdom to ascertain current practice. Eighty-four percent of participants were orthopaedic surgeons and their experience of lumbar spinal fusion ranged from 1-15 years, each performing 4-250 operations in the previous 12 mo. The surgical procedure and patient population is diverse, and it is therefore understandable that management varies. It is evident that care should be patient-centred.
Surgeons consistently saw patients preoperatively, ensured patients are mobile within 3 d of surgery, and valued post-operative physiotherapy. However, variability of protocols, duration of hospital stay, use of discharge criteria, frequency and timing of outpatient follow up, use of written patient information and outcome measures was considerable. Much variability was explained through patient-centred care.
Lumbar spinal fusion surgery aims to fuse two or more vertebrae in the lumbar region using bone or metal implants. The primary indication for lumbar fusion is pain (back and/or leg pain) as a consequence of degenerative disease, where it can potentially stabilise the spine.
It is a well written manuscript concerning survey in the surgical option in lumbar degenerative disorder treated with /without fusion and with/without instruments.
P- Reviewer: Pan HC, Wang Y S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Gibson JN, Waddell G. Surgery for degenerative lumbar spondylosis. Cochrane Database Syst Rev. 2005;CD001352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States’ trends and regional variations in lumbar spine surgery: 1992-2003. Spine (Phila Pa 1976). 2006;31:2707-2714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 687] [Cited by in RCA: 665] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 3. | The Health and Social Care Information Centre. HES online. Primary Diagnosis: 3 character tables [accessed 2011; Oct 20] Available from: http://www.hesonline.nhs.uk. |
| 4. | Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976). 2005;30:1441-1445; discussion 1441-1445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 678] [Cited by in RCA: 729] [Article Influence: 36.5] [Reference Citation Analysis (0)] |
| 5. | Gray DT, Deyo RA, Kreuter W, Mirza SK, Heagerty PJ, Comstock BA, Chan L. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine (Phila Pa 1976). 2006;31:1957-1963; discussion 1964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 223] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 6. | Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259-1265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1141] [Cited by in RCA: 1084] [Article Influence: 72.3] [Reference Citation Analysis (0)] |
| 7. | Katz JN. Lumbar spinal fusion. Surgical rates, costs, and complications. Spine (Phila Pa 1976). 1995;20:78S-83S. [PubMed] |
| 8. | Willems P, de Bie R, Oner C, Castelein R, de Kleuver M. Clinical decision making in spinal fusion for chronic low back pain. Results of a nationwide survey among spine surgeons. BMJ Open. 2011;1:e000391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine (Phila Pa 1976). 2007;32:382-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 351] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 10. | Fairbank J, Frost H, Wilson-MacDonald J, Yu LM, Barker K, Collins R. Randomised controlled trial to compare surgical stabilisation of the lumbar spine with an intensive rehabilitation programme for patients with chronic low back pain: the MRC spine stabilisation trial. BMJ. 2005;330:1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Stromqvist B, Fritzell P, Hagg O, Jonsson B, Sanden B. Follow-up of Lumbar Surgery in Sweden 2007, The Swedish National Spine Register. The Swedish Spinal Surgery Society. Primary Diagnosis: 3 character tables [accessed 2007; [accessed 2011 Sept 26] Available from: http://www.4s.nu/pdf/Ryggregisterrapport_2008_eng_version.pdf. |
| 12. | Rushton A, Wright C, Goodwin P, Calvert M, Freemantle N. Physiotherapy rehabilitation post first lumbar discectomy: a systematic review and meta-analysis of randomized controlled trials. Spine (Phila Pa 1976). 2011;36:E961-E972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | McGregor AH, Dicken B, Jamrozik K. National audit of post-operative management in spinal surgery. BMC Musculoskelet Disord. 2006;7:47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Sim J, Wright C. Research in Health Care: Concepts, Designs and Methods. Stanley Thornes. Cheltenham. 2000;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Wright K. Researching internet-based populations: advantages and disadvantages of online survey research, online questionnaire authoring software packages, and Web survey services. JCMC. 2005;10. [DOI] [Full Text] |
| 16. | Williamson E, White L, Rushton A. A survey of post-operative management for patients following first time lumbar discectomy. Eur Spine J. 2007;16:795-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |